Healthcare in the Year 2030
The Year 2030
by Dr Nick van Terheyden (@DrNic1)
How will the world of medicine change in the next 15 years? Well 15 years ago AOL had just bought Time Warner, the human genome had just been deciphered and published and the first inhabitants of the International Space Station had arrived.
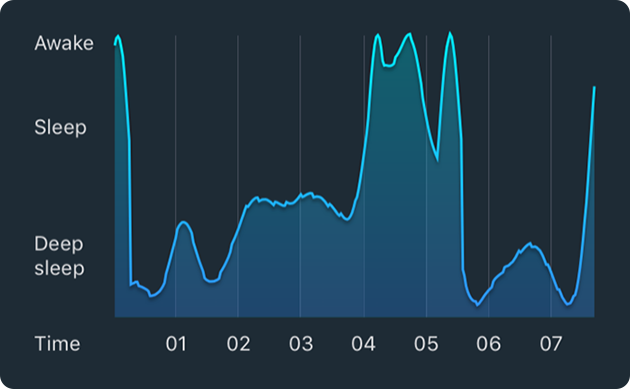
The Year 2030 – my bed has been tracking my vital signs throughout the night and notices I was restless and managed fewer REM cycles during sleep than usual. Prometheus (my personalized artificial automated agent) checks my calendar and traffic and elects to wake me an hour later. Appointments for the morning are rescheduled and my drone pick up is postponed. Prometheus sends an update to “Hestia” (my kitchen AI) with instructions to increase the energy component of my meals for the day to adapt for the lack of sleep and deliver a boost of energy with almond snacks through the day. Prometheus sends my updated sleep and vitals data to my personal health record. While I rest peacefully the rest of the household is awakened and sets about their day.
Time to Get Up
When it’s time to awaken, the bed starts warming to ease the process, the lights slowly turn on and the GPR (Galactic Public Radio) custom news cycle is playing gently in the background. My calendar has been reorganized, and there’s an additional appointment with Asclepius (My health AI) before I leave in the morning. My food is ready and waiting and contains a boost in energy, helping me wake up and acclimate after the poor night’s sleep. I hear the inbound calling for Asclepius and take the call. We review the reasons for my poor night’s sleep and agree I should track this more closely for the next few days to ward off any potential problems. In this instance Asclepius suggests no further investigation is warranted, but if I am worried a drone will be dispatched with some auto investigator tools to apply and track additional parameters if necessary.

As we finish my personal drone arrives and I step outside, catching my foot on a fallen replicator brick discarded by one of the children. As I fall my head strikes the corner of a table and carves into my cheek. Prometheus is immediately on top of the situation checking on my vitals, and while no major damage to my body, the cut will need review and probably some stitches. Checking with local urgent care facilities, the optimal treatment for me today is a quick trip to the urgent care clinic and my drone is reprogrammed to take me there immediately.
Urgent Care in the Future
As I arrive my MedicAlert Digital Bracelet transmits my allergy to lignocaine and identifies me based on the bracelet
and my retinal scan taken as I walk through the door, which authenticates my presence and consent initiates transfer of my medical data and records to the clinic.

I’m guided to a room where a robot nurse cleans my wound and positions me on the bed and brings in the Panacea (the medical repair robot). My medical record shows I have had a recent Tetanus shot, and a comparison of my previous vitals shows there are no serious changes that would warrant additional investigation. Repair completed, my records are updated with the new details and a drone appears to take me to work.
Medical Offices and Care in the Future
As I step into my office my team are all walking in (virtually) and the central console and screens around the room light up with data on our first patient. We process through the details provided by the various Artificial Intelligence agents and data gathering tools. “Jane” (name changed to preserve her privacy) has been having some frequent dizzy spells and falls – her mother had Meniere’s disease and a degenerative disease linked to the A2ML1-AS1 / ADAM20P1 / MTor Complex 2 / WDFY3-AS2 – we think there may be a link. Even though Jane does not have these gene expressions there may be a new epigenetic influencer she received that is affecting her stable sequence. We need to get to the bottom of this. Jane is here too (virtually) – with her mother and father – and they are looking at the same data, shown with basic annotations to help them understand the details.

We think we have an answer, but want to share the details and show Jane and her family the model of the CRISPR editor nanobot and its effects before we decide on the next course of action. Do we create a more realistic model of her body functions with the cell printer and test on that? Or is the confidence in our simulation high enough to warrant immediate therapy? Whatever we decide we will get real time approval from the GMAA (Galactic Medical Agent Agency that replaced the FDA in 2021). Jane and her family have seen a new therapy advertised and they want to understand how that might work for them. We pull up the details and all the data on patients and do an immediate comparison. The data’s questionable but, more importantly, it’s contraindicated in anyone with GRAMS domain, Heat Shock 70kDa protein expression and several others that disqualify Jane.
We elect a wait and see approach – so much easier these days with the real time monitoring and detailed data we have on patients that allows us the scope to wait and watch while reassuring patients. Directives are sent to their family “agents” and a drone dispatched to their location with some additional monitors for Jane to wear to give more detailed data on her for the next few days.

As we complete the consultation a drone arrives with my almond snacks and some water – perfect timing.
This post appeared in abbreviated form on SHIFT communication site – and is included in their downloadable ebook
Healthcare in the Year 2030 was originally published on DrNic1
Population Health is a Team Sport
Designing an Effective Population Health Program
Population health is the topic du jour for the health care industry, and I’m glad to see us all focusing on this important issue. But there is a lot of confusion as to what, exactly, constitutes population health. Or more correctly, an effective population health system.
A good population health program consists of four major components:
- Identification and stratification of risk within a discrete population
- Dissemination of information to physicians, care coordinators or others designated to contact patients and arrange follow up.
- Appropriate follow up to further understand the risks for individual patients, identify gaps in care and design a care plan to help the patient improve his/her health status.
- Ongoing care individualized to each patient’s need. That might be coaching, medication reminders, telehealth visits, remote monitoring or other strategies customized to each person’s condition and socio-economic environment.
The key to making a population health program effective is ensuring that all four components are in place and working well. If there is a break anywhere in the chain, you lose the opportunity to improve patients’ health. The best analytics in the world are useless if the results do not quickly and easily pass into the hands of the people who can take action. And very good follow up and care planning can be ineffective if the ongoing support is lacking.
One of the biggest barriers to effective population health improvement is friction in the flow of information between health plans, hospitals/health systems and physicians. This has been a constant source of difficulty for the entire healthcare ecosystem for years, but with the new focus on population health and improving outcomes, it has reached a new level of urgency.

In traditional African societies coronary artery disease is virtually nonexistent, but in the migrant population to Western societies the rates are similar to those of the local population indicating that the primary determinants of these diseases are lifestyle and diet and not genetic. These indicators are a key asset in changing our healthcare system and addressing the current 75% of our healthcare spending that is focused on patients with chronic conditions which have their roots in lifestyle choices and behaviors. To address these challenges we need a way to better target our limited healthcare resources more cost effectively for maximum effect and identification and targeting with a robust population health system is no longer a nice to have – it’s a must.
To help patients improve their health, not just react to a situation that has already developed, requires information and insights. But in a survey of primary care physicians by The Commonwealth Fund, only 31% of U.S. physicians said they are notified when a patient is discharged from the hospital or seen in an emergency department. This is important information for primary care physicians, and is not that difficult to fix. All you need is standard protocol in place and a mechanism for notification. It could be a standard action that happens at every discharge. It could even be automated. If the retail industry can automatically send an email to confirm an order, hospitals and health systems should be able to send an automatic email to a physician with discharge information. But hospitals and health system executives haven’t made it a priority, so it doesn’t get fixed.
Get to know your team mates
This is just one example of the inward-looking approach that still permeates much of healthcare. Hospitals, nursing homes, skilled nursing facilities and other care providers pay attention to what happens within their organizations, but they neglect to look beyond. Organizations act as though the care they give is the only care patients receive. They forget that there are a multitude of other professionals who are also responsible for care and need to know what’s going on. We don’t just have data silos in healthcare, we have attitudinal silos that make data transfer and exchange an afterthought at best.
It’s like each care provider is a golfer alone on the course and the patient is the ball. As long as that lone golfer moves the ball forward, it’s all good.
The reality is that healthcare is a team sport, more like football (or soccer as it is called in the US) than golf. If you can’t make an accurate, effective pass to your team mates, you lose the ball.

But patients aren’t balls, they’re human beings. When one member of the healthcare team fails to inform the rest of the team, a human being gets lost in the confusion with poor outcomes and frustrated patients.
In population health improvement, you have to play on a team, because it takes a wide variety of skills to make this all happen. And you have to be aware of all the other players on the team. The successful population programs include everyone who is part of the community – not just the healthcare system and resources but all aspects of the community. Dell Medical School held an inaugural event to crowd-source their population health strategy, coming up with areas of focus and metrics for success that included input from a wide range of stake holders. This is the kind of team based approach to population health that will help the whole community win – getting people healthy and staying healthy.
It starts with leadership
Most healthcare organizations are at least partly aware of the problem and are making efforts to solve it. But it is a complex problem, involving, as I noted above, attitudes as well as technology. To make data flow freely to those who need it, you have to have effective technology to integrate, manage and analyze the multitude of data streams in healthcare, and you also need leadership who prioritize data sharing over the competitive interests of conflicting health delivery systems. With free flowing information routed to all the interested parties including the oft forgotten but all important patient, in understandable and actionable form that includes the insights and management options we can successfully identify those at risk and develop appropriate interventions. By including the patient and personal care team that typically includes multiple family members we capitalize on underutilized resources that are both essential and highly effective at improving the trajectory for the patient’s outcome.
Custom Communication and Targeting
Traditional systems and methods have targeted the existing clinical systems and communications which, while suited to some, fail to adapt to the changing world of technology and the fact that people no longer go online – they live online. This doesn’t just apply to patients and their families; it’s increasingly true for clinicians. It can be as simple as a text based reminder for medication, timed to coincide with the patients personal schedule and preferences or as complex as an automated avatar with augmented intelligence that engages with the patient to assess their status and determine the need for additional intervention or personal follow up by the care team.
Each year HealthIT week raises awareness of technology in healthcare, bringing together innovators and key healthcare leaders who are diligently working together to make the best use of information technology to improve the healthcare systems and ultimately our each and everyone’s individual health. This past year we lost one of the titans whose personal journey of uncoordinated care she shared in her attempt to correct the system – Jess Jacobs (#UnicornJess). It might be too late for Jess but let this be the year we move past the individual approach in healthcare driven by underlying economics and focus on the team sport of population health and democratize access to the best possible care and outcomes to the widest swathe of people…worldwide.
This post originally appeared here
Population Health is a Team Sport was originally published on DrNic1
FDA clears sound wave technology to blas
FDA clears sound wave technology to blast plaque in arteries http://ow.ly/a0rZ504B5LK
Infographic: 5 Kinds of Mobile Health Us
Infographic: 5 Kinds of Mobile Health Users http://ow.ly/A9v3504B5LJ
Here’s how #wearables are being enlisted
Here’s how #wearables are being enlisted to study neurodegenerative diseases http://ow.ly/EtaT504B5LH
leave a comment