Giving Personal Health Advice to Family and Friends
In an interesting post on the medscape site (subscription/registration probably required): The Pitfalls of Giving Free Advice to Family and FriendsShelly Reese described some of the challenges of giving medical advice
to friends and family (even if you are a wannabe Dr Phil).
As she puts it the path can sometimes lead to challenging areas of ethics and professional boundaries.
How do you address or deflect such requests? Unfortunately, there are no easy answers. It depends a lot on you, your boundaries, and the situation.
And she links to the AMA Guidelines
The American Medical Association (AMA) Code of Medical Ethics is clear, however: “Physicians generally should not treat themselves or members of their immediate families.”[1] The statement goes on to provide an extensive list of good reasons why, including personal feelings that may unduly influence medical judgment, difficulty discussing sensitive topics during a medical history, and concerns over patient autonomy (Ref: American Medical Association. Code of Medical Ethics Opinion 8.19: Self-treatment or treatment of immediate family members. Issued June 1993.)
Some of the challenges of simple advice include
- Escalation to more complex or persistent advice
- Long distance diagnosis with missing data
- Lack of Doctor/Patient relationship and documentation
- Litigation
- Impaired judgement
- Changing and coloring of relationships
In one section she describes the challenges of dealing with family members and says
“I try not to give too much medical advice, even to my parents. I see my role as an advocate: to help them synthesize information when they have questions. When my mother calls and says, ‘I’m short of breath and I don’t know what to do,’ I walk her through all the things her doctor has talked to her about: Have you taken your blood pressure and pulse? Do you know how many times you’re breathing per minute?”
Good advice on being the patient advocate and healthcare manager for your family members (which many already are) In the end it boils down to personal judgement and your own boundaries.
Questions are appropriate and to be expected, Caplan says, but doctors have to wrestle with themselves in determining how to respond if they’re to act responsibly and ethically. “When close friends and family ask for medical advice, that’s always a matter for introspection, and at the end of the day, it’s not resolved by codes of ethics but by considered individual judgments.”
It used to be as the trusted source of knowledge where access to information was limited this was a significant responsibility but with the age of
and medical applications like AskMD, iTriage and HealthTap to mention a few you might find there is fewer and fewer requests. So for those of you that like the opportunity to help others out…enjoy it while you can mHealth and Telemedicine may be changing the landscape and soon!
Google Glass in Healthcare – Part 1 the Basic Facts
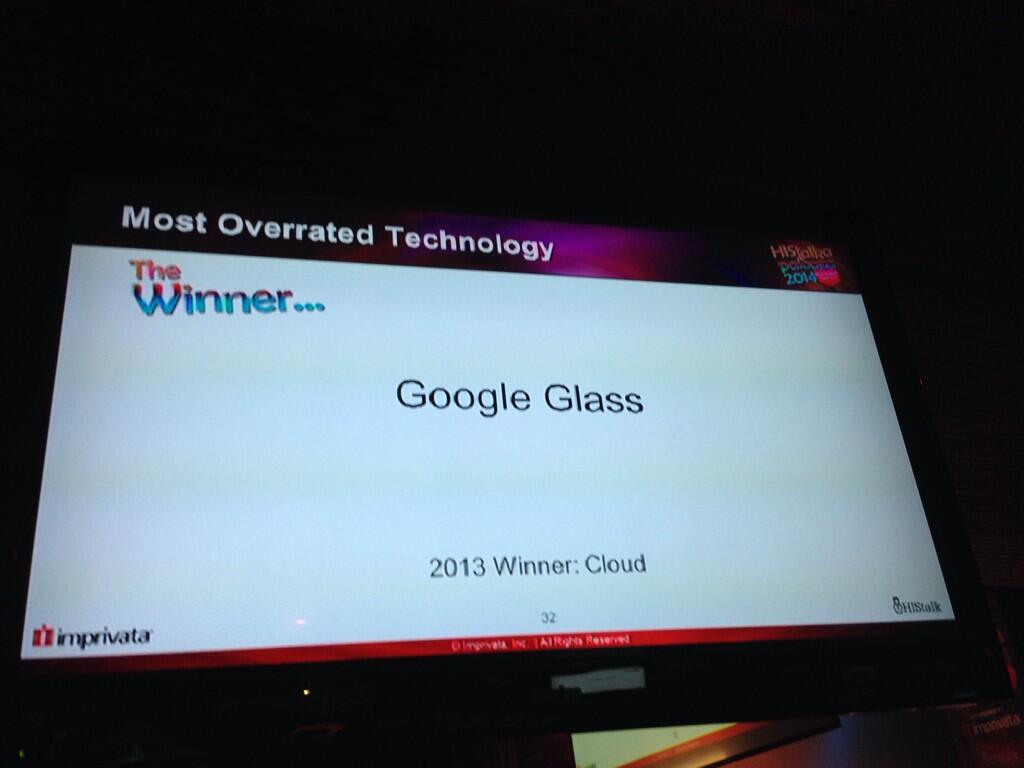
HIMSS was exciting and despite the HIS Talk HISies awarding Google Glass the most over rated technology:
Oh, @wareflo – this could hurt… #HIStalkapalooza14 Most overrated tech @histalk HISSIES #HIMSS14 pic.twitter.com/dThovzVWvo — Mandi Bishop (@MandiBPro) February 25, 2014
I know I am biased as one of the lucky Google Glass Explorer as can be seen in this post from MedCity Watching for Wearables at #HIMSS14:
I think they are wrong and its not just Glass that will provide better more ready access to essential clinical data.
Not to say that the initial program like many launches have had their problems with early releases of technology not quite ready for prime time – remember the 1987 Apple Newton:
Even the omnipresent iPad struggled initially – most have probably forgotten the initial lukewarm reception of the iPad
had Apple talking about a price reduction.
Mat Honan (one on the same “Epic Hack”) wrote a piece about his early experiences “My Year with Google Glass” that highlighted some early acceptance challenges
- Glass is socially awkward
- People get angry at Glass
- Wearing Glass separates you
and I would add Glass interrupts normal conversations and social behavior – but that is all now and like the mobile phone I believe it will be come a natural part of our technical fabric. Think back to 2007 and how pulling out a phone in a meeting was frowned upon – now it seems part of the fabric of many of the meetings I attend. But it was Mat’s commentary on the impact it had on his perception fo phones that really stuck out for me
Glass kind of made me hate my phone — or any phone. It made me realize how much they have captured our attention. Phones separate us from our lives in all sorts of ways. Here we are together, looking at little screens, interacting (at best) with people who aren’t here. Looking at our hands instead of each other. Documenting instead of experiencing.
Which resonates with me an the Art of Medicine campaign and the struggle clinicians have with focusing on the patient (To learn more, download the eGuide Art of Medicine in a digital world). As Dr. Edward C. Grendys, Jr. said in his article: There’s no room for technology in end-of-life care decisions:
From initial diagnosis through to surgical therapies, chemotherapy treatments and even end-of-life care, my job is to listen, assess and provide educated decisions that ultimately impact the health and wellness of another human being…. it’s my belief that when talking face-to-face with a patient about a care plan aimed at eradicating their body of a disease that threatens to take them away from their family, there’s no room for paper, computers and/or mobile devices. In these most intimate of conversations, the focus has always and must remain on the communication between the caregiver and the patient on the receiving end. That, in its purest essence, is what practicing the art of medicine is truly all about.
That’s not to say that Google Glass can solve this problem and in its current state and acceptance it might cause more challenges – but the potential is there to blend information access and capture into a physician patient interaction that remains all about the patient
Glass will provide improved access to essential clinical data to clinicians but as my friend Chuck Webster has pointed out on several occasions this is not just for clinicians. Patients are already accessing the internet in droves for clinical information, researching their conditions and that of their relatives and communities abound with resources and support for conditions from common to rare.
Before talking about some of the potential medical applications it is worth detailing the technology. Google Glass is basically a computer with 12Gb of memory attached to your head in the form of glasses. It has a heads up display with voice activation and has some apps that can be installed:
Facts
- Google Glass is basically a computer attached to a pair of glasses
- Google Glass has a display that is projected in front of the Right Eye that is a high resolution display equivalent of a 25 inch high definition screen from eight feet away
- Google Glass has a camera that points forward and can take pictures (5MP) or video (720p) that is closely aligned with the view you see from your own eyes
- Google Glass is voice activated using speech recognition to interact with the glass computer
- Google Glass works best when connected to the internet
- Google Glass Integrates with an Andorid Phone with a limited set of functions available for the iPhone
- Google Glass has no built in illumination so pictures or video taken in dark conditions do not work well
- The screen can be hard to see in bright light
There are many myths circulating:
Myths
- If someone is wearing Google Glass they are recording me
- False – The device is not set up to record continuously and will only record a video or photo based on an action by the wearer (either a spoken request
- OK Glass, take a picture
- or by pressing a button on the google glass device
- Once Someone Has recorded something on Google Glass it is Publicly Posted
- False – it requires an action on the part of the Glass owner to post the material to the internet otherwise it resides on the Google Glass device. It will be synchronized with the users Google+ account for automatic backup (much like photos are backed up from the iPhone to iCloud but like iCloud remain private to the user unless they elect to share them)
- Google Glass is constantly capturing data and transmitting it to the Internet
- False. Without an internet connection Google Glass simply stores any recorded information in the glass memory. And unless you have set it to record there is no data being captured
- Google Glass tracks users and unsuspecting bystanders
- False – Google Glass is not tracking or recording anything unless instructed to do so by the user
So who is using this technology, where are they using it and how are they using it in Healthcare. This articlecovered some of the early concepts and featured a short list of potential applications
- Video sharing and storage: Physicians could record medical visits and store them for future reference or share the footage with other doctors.
- A diagnostic reference: If Glass is integrated with an electronic medical record (EMR), it could provide a real-time feed of the patient’s vital signs.
- A textbook alternative: Rather than referring to a medical textbook, physicians can perform a search on the fly with their Google Glass.
- Emergency room/war zone care: As storied venture capitalist Marc Andreessen proposed in a recent interview, consider ”dealing with wounded patients and right there in their field of vision, if they’re trying to do any kind of procedure, they’ll have step-by-step instructions walking them through it.” In a trauma situation, doctors need to keep their hands free.
- Helping medical students learn: As suggested by one blogger, a surgeon might live stream a live — and potentially rare — surgery to residents and students.
- Preventing medical errors: With an electronic medical record integration, a nurse can scan the medication to confirm whether it’s the correct drug dose and right patient
In its simplest form just transmitting images in real time can offer some advantages for diagnosis – in Rhode Island they are planning on implementing Google Glass for the ED doctors to obtain real time consults with dermatologists.
And this from Kareo showing a patient education application that records the physician patient interaction and then makes it available afterwards for additional review:
In this case featured in the ER doctors use Google Glass and QR codes to identify patients which featured Dr. John Halamka, CIO of Beth Israel Deaconess Medical Center which he talked about in his blog detailing their experience (oddly the articletalking about this refers to text that appears to have been changed or taken down):
When a clinician walks into an emergency department room, he or she looks at [a] bar code (a QR or Quick Response code) placed on the wall. Google Glass immediately recognizes the room and then the ED Dashboard sends information about the patient in that room to the glasses, appearing in the clinician’s field of vision. The clinician can speak with the patient, examine the patient, and perform procedures while seeing problems, vital signs, lab results and other data.
And this concept by the way was top of everyone’s wish list that I talked to in my unofficial survey of engaged and interested observers of my own pair. I’ll paraphrase
If I could get it to recognize someone and provide me with their name when I meet them that would be fantastic!
But it is in urgent care where there is so much potential:
This recent piece on Healium featured in the Seattle King5 News Station: Seattle Doctor testing Google Glass for Surgery in the ER (click on the link if the video does not show below to see it in action)
“If I want to look at for example radiology I can double tap ‘radiology…There’s his chest x-ray, it just popped up, oh he’s got a middle lobe pneumonia”
Part 2 will cover medical applications and how Google Glass technology can be applied in a busy clinical setting
Comments Off on Google Glass in Healthcare – Part 1 the Basic Facts









leave a comment